Health disparities/equity
E-Poster Available
(198) Comparative outcomes for transgender patients: Gaps in HIV pre-exposure prophylaxis (PrEP) adoption between transgender and cisgender individuals.
Wednesday, October 29, 2025
Scott M. Myers, MBA
PearlDiver Technologies
Colorado Springs, Colorado, United StatesScott M. Myers, MBA
PearlDiver Technologies
Colorado Springs, Colorado, United States
Presenter(s)
Primary Author(s)
Background: : Health challenges facing the transgender population differ from those of the cisgender population. There has been minimal research using large national claims databases to investigate such health disparities.
Objective: : Using a large, national, all-payer database, a study was designed to investigat gaps in the adoption of PrEP among the transgender community in relation to adoption rates with the cisgender population.
Methods: : Utilizing the Mariner170 all-payer national claims database, the transgender cohort was defined as patients with ≥1 claim of gender identity disorder occurring between January 2010 and April 2023 using ICD-9 and ICD-10 codes. Propensity score matching was performed against a control group. T-tests and chi-square tests were used to compare the transgender cohort to the cisgender cohort across 32 comorbidities. Patients must have ≥ 2 outpatient claims or ≥1 inpatient claim of each respective comorbidity to be considered a member of the comorbidity cohort. Patient age at first appearance in the database was used.
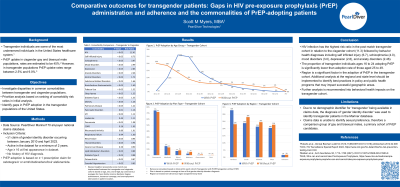
Results: : Within the database, 71,741 individuals with ≥1 ICD9 or ICD10 diagnosis for gender identity disorder (ICD9 302.50:302.53, 302.6, 302.85, ICD10 F64.0:F64.9, Z87.890) as a method of identifying transgender individuals. The highest risk ratio among attributes studied was HIV (12.4) followed by self-inflicted injuries (10.3), schizophrenia (5.1), and mood disorders (4.3) for the transgender population.
The rate of transgender patients with no HIV diagnosis having ≥ 1 claim for PrEP is 5.2% (3,567/68,725). This is significantly lower than national estimates of 35-45% adoption among the high-risk group of gay males. An analysis of the cisgender adopters of PrEP was performed to identify key indicators of PrEP adoption. A logistic regression was performed to identify contributing factors to adopting PrEP. Age was confirmed to be a significant factor, with a t-test confirming significance in difference of mean age between the groups (31.4, 40.3).
Conclusions: : The adoption rate of PrEP in the transgender community aged ≥16 without a diagnosis for HIV (3,058/45,024) is significantly lower than rates among other high-risk populations. It is recommended further research be conducted concerning this gap in treatment and that targeted programs be implemented to increase PrEP adoption rates in the transgender community.
Sponsorship:: PearlDiver Technologies
